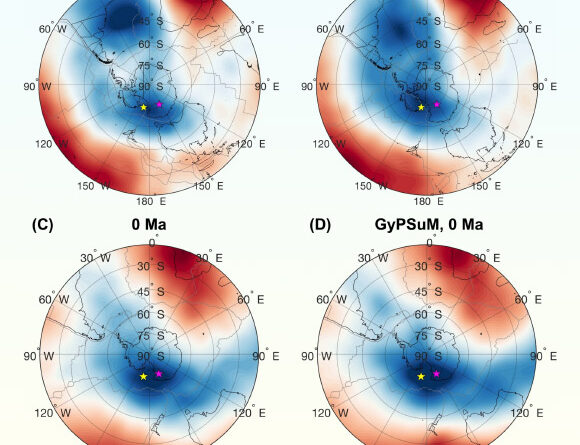
(Image credit: wildpixel through Getty Images)
Envision going to the healthcare facility for a bacterial ear infection and hearing your medical professional state, “We’re out of choices.” It might sound significant, however antibiotic resistance is pressing that circumstance more detailed to ending up being truth for an increasing variety of individuals. In 2016, a lady from Nevada passed away from a bacterial infection that was resistant to all 26 prescription antibiotics that were offered in the United States at that time.
The U.S. alone sees more than 2.8 million antibiotic-resistant health problems each yearInternationally, antimicrobial resistance is connected to almost 5 million deaths each year
As resistant germs spread out, lifesaving treatments deal with brand-new problems — typical infections end up being harder to deal with, and regular surgical treatments end up being riskier. Slowing these hazards to contemporary medication needs not just accountable antibiotic usage and great health, however likewise awareness of how daily actions affect resistance.
Given that the creation of prescription antibiotics in 1910 with the intro of Salvarsana miracle drug utilized to deal with syphilis, researchers have actually been sounding the alarm about resistanceAs a microbiologist and biochemist who research studies antimicrobial resistanceI see 4 significant patterns that will form how we as a society will challenge antibiotic resistance in the coming years.
1. Faster diagnostics are the brand-new cutting edgeFor years, dealing with bacterial infections has included a great deal of informed uncertaintyWhen a really ill client comes to the health center and clinicians do not yet understand the precise germs triggering the health problem, they typically begin with a broad-spectrum antibioticThese drugs eliminate several kinds of germs simultaneously, which can be lifesaving– however they likewise expose a vast array of other germs in the body to prescription antibiotics. While some germs are eliminated, the ones that stay continue to increase and spread resistance genes in between various bacterial types. That unneeded direct exposure provides safe or unassociated germs a possibility to adjust and establish resistance.
On the other hand, narrow-spectrum prescription antibiotics target just a little group of germs. Clinicians usually choose these kinds of prescription antibiotics since they deal with the infection without troubling germs that are not associated with the infection. It can take numerous days to recognize the specific germs triggering the infection. Throughout that waiting duration, clinicians frequently feel they have no option however to begin broad-spectrum treatment– specifically if the client is seriously ill.
Get the world’s most remarkable discoveries provided directly to your inbox.

Amoxicillin is a frequently recommended broad-spectrum antibiotic. (Image credit: TEK IMAGE by means of Getty Images)Brand-new innovation might fast-track recognition of bacterial pathogens, permitting medical tests to be carried out right where the client is rather of sending out samples off-site and waiting a very long time for responses. In addition, advances in genomic sequencing microfluidics and expert system tools are making it possible to determine bacterial types and reliable prescription antibiotics to combat them in hours instead of days. Predictive tools can even prepare for resistance development
For clinicians, much better tests might assist them make faster medical diagnoses and more reliable treatment strategies that will not intensify resistance. For scientists, these tools indicate an immediate requirement to incorporate diagnostics with real-time monitoring networks efficient in tracking resistance patterns as they emerge.
Diagnostics alone will not resolve resistance, however they supply the accuracy, speed and early caution required to remain ahead.
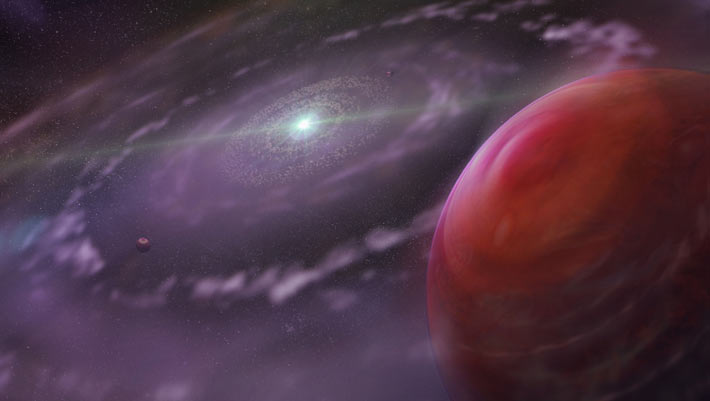
2. Broadening beyond conventional prescription antibioticsPrescription antibiotics changed medication in the 20th centuryhowever counting on them alone will not bring humankind through the 21st. The pipeline of brand-new prescription antibiotics stays distressingly thin, and a lot of drugs presently in advancement are structurally comparable to existing prescription antibiotics, possibly restricting their efficiency.The antibiotic discovery space
Due in part to an absence of monetary reward for the pharmaceutical market to purchase antibiotic advancement, there has actually not been a brand-new class of prescription antibiotics considering that 1987. (Image credit: Chart: The Conversation, CC-BY-ND Source: ReAct Group Get the information)To remain ahead, scientists are buying nontraditional treatments, much of which operate in essentially various methods than basic prescription antibiotics.
One appealing instructions is bacteriophage treatmentwhich utilizes infections that particularly contaminate and eliminate hazardous germs. Others are checking out microbiome-based treatments that bring back healthy bacterial neighborhoods to crowd out pathogens.
Scientists are likewise establishing CRISPR-based antimicrobialsutilizing gene-editing tools to exactly disable resistance genes. New substances like antimicrobial peptideswhich pierce the membranes of germs to eliminate them, reveal guarantee as next-generation drugs. Researchers are creating nanoparticle shipment systems to transfer antimicrobials straight to infection websites with less adverse effects.
Beyond medication, researchers are analyzing eco-friendly interventions to minimize the motion of resistance genes through soil, wastewater and plasticsalong with through waterways and essential ecological tanks.
A number of these alternatives stay early-stage, and germs might ultimately develop around them. These developments show an effective shift: Instead of wagering on finding a single antibiotic to attend to resistance, scientists are developing a more varied and durable tool package to combat antibiotic-resistant pathogenic germs.
3. Antimicrobial resistance outside medical facilitiesAntibiotic resistance does not just spread out in medical facilities. It moves through individuals, wildlife, crops, wastewater, soil and international trade networks. This more comprehensive point of view that takes the concepts of One Health into account is vital for comprehending how resistance genes take a trip through environments.
Scientists are progressively acknowledging ecological and farming aspects as significant chauffeurs of resistance, on par with abuse of prescription antibiotics in the center. These consist of how prescription antibiotics utilized in animal farming can develop resistant germs that infect individuals; how resistance genes in wastewater can endure treatment systems and go into rivers and soil; and how farms, sewage plants and other ecological locations end up being centers where resistance spreads out rapidly. Even worldwide travel speeds up the motion of resistant germs throughout continents within hours.
The Trouble with Antibiotics (complete documentary)|FRONTLINE – YouTube
See On
Together, these forces reveal that antibiotic resistance isn’t simply a problem for health centers– it’s an environmental and social issue. For scientists, this implies developing services that cross disciplines, incorporating microbiology, ecology, engineering, farming and public health.4. Policies on what treatments exist in the futureDrug business lose cash establishing brand-new prescription antibioticsSince brand-new prescription antibiotics are utilized moderately in order to protect their efficiency, business typically offer too couple of dosages to recover advancement expenses even after the Food and Drug Administration authorizes the drugs. A number of antibiotic business have actually declared bankruptcy for this factor.
To motivate antibiotic development, the U.S. is thinking about significant policy modifications like the PASTEUR ActThis bipartisan costs proposes producing a subscription-style payment design that would enable the federal government as much as US$ 3 billion to pay drug producers over 5 to 10 years for access to crucial prescription antibiotics rather of paying per tablet.
International health companies, consisting of Médecins Sans Frontières (Doctors Without Borders), care that the costs must consist of more powerful dedications to stewardship and fair gain access to
Still, the expense represents among the most considerable policy propositions associated with antimicrobial resistance in U.S. history and might identify what prescription antibiotics exist in the future.
The future of antibiotic resistanceAntibiotic resistance is often framed as an inescapable disaster. I think the truth is more enthusiastic: Society is going into a period of smarter diagnostics, ingenious treatments, ecosystem-level techniques and policy reforms intended at reconstructing the antibiotic pipeline in addition to resolving stewardship.
For the general public, this indicates much better tools and more powerful systems of defense. For scientists and policymakers, it indicates teaming up in brand-new methods.
The concern now isn’t whether there are services to antibiotic resistance– it’s whether society will act quick enough to utilize them.
This edited short article is republished from The Conversation under a Creative Commons license. Check out the initial post
The significant styles of research study in the Hudson laboratory are vested in biochemistry and microbiology. More particularly, in the locations of amino acid metabolic process, structural analyses of enzymes associated with amino acid and bacterial peptidoglycan metabolic process that are putative targets for antibiotic advancement, and the seclusion, recognition and genomic characterization of plant-associated germs. Dr. Hudson has actually protected roughly $3 million in federal/state financed grants and agreements as PI and or CoPI from the NIH, NSF, Bayer Corporation, Sweetwater Energy and Natcore Technology. Dr. Hudson has actually released over 75 peer-reviewed short articles.
Dr. Hudson is an extremely appreciated and well liked instructor. His mentor contributions are significant specifically throughout the conversion to terms when he reworded all the courses he teaches. Dr. Hudson has actually mentored and engaged lots of trainees in research study and has actually released in peer-reviewed journals with a variety of them. Much of his trainees have actually gone to pursue more research study at distinguished organizations. Dr. Hudson signed up with the RIT professors in 2008 following a post-doctoral fellowship at Rutgers University. He made his B.S. (2000) in Biology from Virginia Union University, Richmond, VA., and his Ph.D. (2006) in Plant Biochemistry from Rutgers University.
You need to validate your show and tell name before commenting
Please logout and after that login once again, you will then be triggered to enter your display screen name.
Learn more
As an Amazon Associate I earn from qualifying purchases.