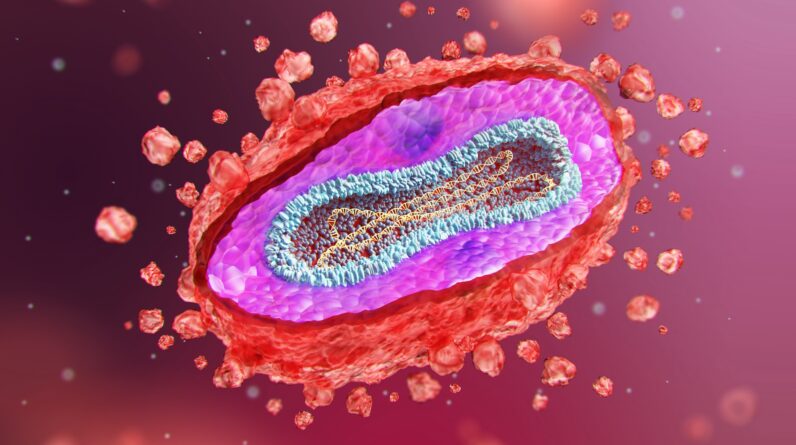
(Image credit: SERGII IAREMENKO/SCIENCE PHOTO LIBRARY via Getty Images)
Editor’s note: Following the publication of this article, Sweden reported the first known case of clade 1 mpox outside of Africa on Aug. 15.
The mounting mpox outbreak in Africa constitutes a public health emergency of international concern, the World Health Organization (WHO) declared Wednesday (Aug. 14).
The declaration hinged on advice from an emergency committee that the WHO assembled to discuss an unprecedented surge of mpox in the Democratic Republic of the Congo (DRC), which has now spilled into adjacent countries. Mpox cases were already rising in the DRC in 2023, but now they’ve skyrocketed — more than 14,000 cases have been reported so far in 2024, exceeding last year’s total count.
“In the view of all members, it was unanimous that the current outbreak of mpox is an extraordinary event,” Dr. Dimie Ogoina, a physician-scientist and the chair of the 15-member emergency committee, said during a virtual news conference on Wednesday. One big factor in the decision was that “we’re having the highest number of cases ever reported in the DRC,” he said.
Based on the available data, children in the DRC have been the “worst impacted” by the country’s outbreak, Ogoina said. That seems to be the case in Burundi, as well, but not in Nigeria and South Africa, where so far young adults have been most impacted. That said, health officials don’t yet understand the full extent of the emergency in the DRC or elsewhere in Africa.
Related: ‘Mpox’ is the new name for monkeypox, the WHO says
“What we have in Africa is actually the tip of the iceberg,” Ogoina said, citing major gaps in diagnostic testing. “We don’t have the full picture of this burden of mpox.”
Mpox poses a particularly high risk in Africa due to the continent’s high burden of HIV infections, a percentage of which are undiagnosed or undertreated. People living with HIV, and especially those with advanced disease, face a higher risk of severe illness and death from mpox, Ogoina said.
Another factor in the committee’s decision was the fact that a new branch of the mpox virus family tree, called clade 1b, has emerged. It was first spotted in the DRC last year and has since spread to bordering countries where mpox had not previously been reported. These countries include Burundi, Kenya, Rwanda and Uganda.
“But we are not dealing with one outbreak of one clade,” WHO Director-General Dr. Tedros Adhanom Ghebreyesus said in his opening remarks to the emergency committee. “We are dealing with several outbreaks of different clades in different countries with different modes of transmission and different levels of risk.”
There are two major clades of mpox, known as clade 1 and clade 2, and the former carries a higher risk of severe disease and death than the latter. Clade 1 viruses have never been detected beyond countries where mpox regularly spreads. (The mpox outbreak that spread to many countries, including the U.S., in 2022 was driven by a clade 2 virus.)
This year, two offshoots of clade 1 — called 1a and 1b — have been circulating in various African countries, and both are spreading in the DRC. In addition, clade 2 viruses have been spreading in several countries, such as Cameroon, Nigeria and South Africa.
The picture of how mpox is spreading is complex. The main mode of transmission is through close physical contact, which drives spread in households, for instance, said Maria Van Kerkhove, the WHO’s acting interim director of Epidemic and Pandemic Preparedness and Prevention (EPPP). The virus, and especially clade 1b, is also spreading through sexual networks. To a lesser extent, transmission from contact with infected animals or their bodily fluids is also driving cases, she added.
In the DRC and Burundi, there’s evidence that mpox is spreading through community networks, Dr. Abou Salam Gueye, the emergency director for the WHO African Region, said at the news conference. But in some other countries that have reported fewer cases, such as Kenya, Uganda and Côte d’Ivoire, it’s suspected that these cases have been isolated events, he said.
The WHO is now working to increase the availability of mpox vaccines in Africa by securing deals with manufacturers and donations from countries with existing stockpiles. They’re working with the makers of vaccines called MVA-BN (which is marketed as Jynneos in the U.S.) and LC16, which is produced by the government of Japan, according to Tim Nguyen, head of the Unit for High Impact Events within the EPPP department.
“Vaccines are one intervention that can be utilized,” Van Kerkhov said. But there’s also work that needs to be done around communicating people’s risk of mpox and precautions that can be taken to prevent the disease, she added.
In addition, more studies need to be undertaken to understand how the virus’ transmission dynamics differ in different settings and how illnesses from mpox progress, and as Ogoina noted, gaps in testing need to be closed, she said.
Without swift action, mpox could spread to additional African countries and also beyond the continent.
As such, “mpox requires a coordinated response, not only in Africa, but globally,” Ogoina said. “Collectively, all parties involved can work to improve surveillance, diagnosis, and other public health responses that are needed to nip this challenge in the bud.”
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line “Health Desk Q,” and you may see your question answered on the website!
As an Amazon Associate I earn from qualifying purchases.