(Image credit: Christian Keenan through Getty Images)
FAST FACTS
Turning point: Individual contaminated with SARS
Date: Nov. 16, 2002[19659007]Where: Foshan, China
Who: A food handler
In January 2003, epidemiologists in China recognized 2 cases of “atypical pneumonia” in clients who had actually checked out healthcare employees in Guangdong province. Groups started contact tracing and ultimately found that the bacterium accountable for the health problems had actually been flowing considering that a client fell ill Nov. 16, 2002.
Those early cases in November remained in “food handlers” — those who either worked as chefs in dining establishments or as suppliers at “wet markets,” where live animals, such as poultry and more-exotic animals like civet felines and raccoon pet dogs, were kept in congested conditions.
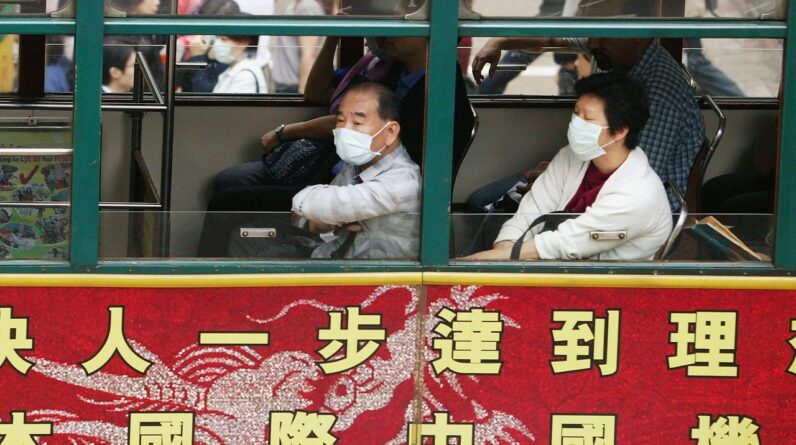
By the time Chinese illness private investigators recognized a break out may be unfolding, the illness had actually currently been flowing for 2 months and had actually infected healthcare employees.The illness reached Hong Kong in February and after that blew up when a nephrologist from southern China taken a trip to the area for a wedding event on Feb. 21, 2003. He was weak throughout his journey and later on passed away of the illness.
In March, a case private investigator for the World Health Organization (WHO), Dr. Carlo Urbani, pertained to examine a case observed in a business person who had actually taken a trip to Hong Kong before showing up in Hanoi, Vietnam, and being hospitalized there. Urbani eventually got the illness himself and passed away that very same month
By March 12, the WHO had actually released an alert about a extreme type of pneumonia of unidentified origin in individuals from China, Hong Kong and Vietnam. By March 15, the Centers for Disease Control and Prevention (CDC) had actually formally called the illness serious intense breathing syndrome (SARS), and by March 24they had actually determined an unique coronavirus as the cause.
Dr. Carlo Urbani was a WHO doctor who passed away while examining the SARS epidemic. (Image credit: HOANG DINH NAM by means of Getty Images)By that time, the break out had neared its peak. The pandemic lasted for months, infected 28 nations beyond China– with 29 cases in the U.S.– and impacted more than 8,000 individuals, 774 of whom passed awayThe illness’s case-fatality rate was approximated to be around 9.6 %.
Get the world’s most remarkable discoveries provided directly to your inbox.
In early 2004, SARS briefly flared once again, however its spread was rapidly squelched through an aggressive and fast contact-tracing-and-containment method.
That 2nd flare-up allowed researchers to trace the SARS infection to palm civets and raccoon pet dogs cost markets. The next year, researchers proposed that horseshoe bats were the pathogen’s initial animal host, however it wasn’t up until 2017 that scientists discovered the smoking cigarettes weapon: bats bring an abundant swimming pool of SARS-like infections residing in remote collapse China’s Yunnan provinceThe caverns were simply a mile far from towns.
“The risk of spillover into people and emergence of a disease similar to SARS is possible,” authors warned in their paper at the time.
The SARS epidemic, as scary as it was at the time, was ultimately just a dress rehearsal for the COVID-19 pandemic that swept across the globe from March 2020 to May 2023, after early cases started to emerge in November 2019. The two viruses belong to the same general family of coronaviruses and likely emerged from a similar animal host.
Scientists and public health officials successfully applied some of the lessons of SARS to the COVID pandemic. For instance, when SARS first emerged, China had a very rudimentary infectious-disease surveillance system. While they did report cases of infectious and food-borne diseases, communication was by telephone call, there was no standardized case reporting system, and they had no system in place to track contacts or collect lab results. After the SARS epidemic, China quickly implemented a thorough contact-tracing and disease-surveillance system.
Palm civets from a market evaluated favorable for SARS throughout the epidemic. (Image credit: Rangga ozi bayu permana through Getty Images)
That would show essential when SARS-CoV-2, the coronavirus that triggers COVID-19, emerged in China. The nation logged numerous countless cases of infections throughout the very first wave, which ended in China by mid-February– simply a couple of months after detectives initially reported a cluster of pneumonia cases of unidentified cause in Wuhan. (A heavy-handed lockdown likewise likely assisted consist of the infection’s spread within the nation.)
Whereas it took months to determine the reason for the SARS pandemic, the SARS-CoV-2 infection was determined less than 2 weeks after the very first cases were seen. And SARS had no particular treatment, whereas by mid-March 2020, vaccines versus the recently determined infection remained in medical trials, thanks to mRNA innovation that had actually remained in the works for years
Other lessons the world might have drawn from SARS were just partly discovered. In 2017, when the SARS source was recognized, Dr. Kwok-Yung Yuena virologist at the University of Hong Kong who co-discovered the infection, informed Nature News that the finding “reinforces the notion that we should not disturb wildlife habitats and never put wild animals into markets.” He informed Nature News that appreciating nature “is the way to stay away from the harm of emerging infections.” The practice continued.
In some methods, the SARS epidemic likewise offered public health companies an incorrect complacency. SARS and associated coronavirus illness, such as Middle East breathing syndrome (MERS), were much deadlier than SARS-CoV-2 however likewise a lot easier to consist of. Break outs were fairly simple to control utilizing contact tracing and other public health steps, instead of needing the circulation of vaccines.
That’s since SARS had a much shorter transmittable window than COVID-19. It was most contagious throughout the 2nd week of the health problem, when individuals were seriously ill, whereas SARS-CoV-2 was quickly sent from the early stages of illnessin some cases even before signs emerged.
Tia is the handling editor and was formerly a senior author for Live Science. Her work has actually appeared in Scientific American, Wired.com and other outlets. She holds a master’s degree in bioengineering from the University of Washington, a graduate certificate in science composing from UC Santa Cruz and a bachelor’s degree in mechanical engineering from the University of Texas at Austin. Tia belonged to a group at the Milwaukee Journal Sentinel that released the Empty Cradles series on preterm births, which won several awards, consisting of the 2012 Casey Medal for Meritorious Journalism.
Learn more
As an Amazon Associate I earn from qualifying purchases.