Tiny chips can be powered by infrared light if they’re near the brain’s surface area.
An immune cell chemically connected to a CMOS chip.
Credit: Yadav, et al.
Basic brain implants utilize electrodes that permeate the noodle to promote and tape the activity of nerve cells. These normally require to be put in location by means of a surgery. To walk around that requirement, a group of scientists led by Deblina Sarkar, an electrical engineer and MIT assistant teacher, established tiny electronic gadgets hybridized with living cells. Those cells can be injected into the circulatory system with a basic syringe and will take a trip the blood stream before implanting themselves in target brain locations.
“In the very first 2 years of dealing with this innovation at MIT, we’ve got 35 grant propositions declined in a row,” Sarkar states. “Comments we obtained from the customers were that our concept was extremely impactful, however it was difficult.” She acknowledges that the proposition seemed like something you can discover in sci-fi books. After more than 6 years of research study, she and her coworkers have actually pulled it off.
Nanobot issues
In 2022, when Sarkar and her associates collected preliminary information and got some appealing outcomes with their cell-electronics hybrids, the group proposed the job for the National Institutes of Health Director’s New Innovator Award. For the very first time, after 35 rejections, it made it through peer evaluation. “We got the greatest effect rating ever,” Sarkar states.
The factor for that rating was that her innovation resolved 3 incredibly tough issues. The very first, undoubtedly, was making practical electronic gadgets smaller sized than cells that can flow in our blood.
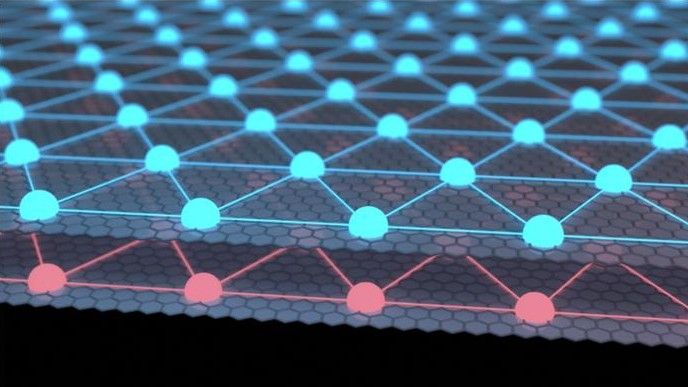
“Previous expeditions, which had actually not seen a great deal of success, depended on putting magnetic particles inside the blood stream and after that directing them with electromagnetic fields,” Sarkar discusses. “But there is a distinction in between electronic devices and particles.” Electronic devices used CMOS innovation (which we utilize for making computer system processors) can create electrical power from inbound light in the very same method as photovoltaics, in addition to carry out calculations essential for more smart applications like picking up. Particles, on the other hand, can just be utilized to promote cells to a level.
If they ever reach those cells, obviously, which was the 2nd issue. “Controlling the gadgets with electromagnetic fields indicates you require to enter into a device the size of an MRI,” Sarkar states. As soon as the topic remains in the device, an operator takes a look at where the gadgets are and attempts to move them to where they require to be utilizing absolutely nothing however electromagnetic fields. Sarkar stated that it’s hard to do anything besides move the particles in straight lines, which is a bad match for our really complicated vasculature.
The service her group discovered was merging the electronic devices with monocytes, immune cells that can home in on swelling in our bodies. The concept was that the monocytes would bring the electronic devices through the blood stream utilizing the cells’ chemical homing system. This likewise fixed the 3rd issue: crossing the blood-brain barrier that secures the brain from pathogens and contaminants. Electronic devices alone might not survive it; monocytes could.
The difficulty was making all these concepts work.
Clicking together
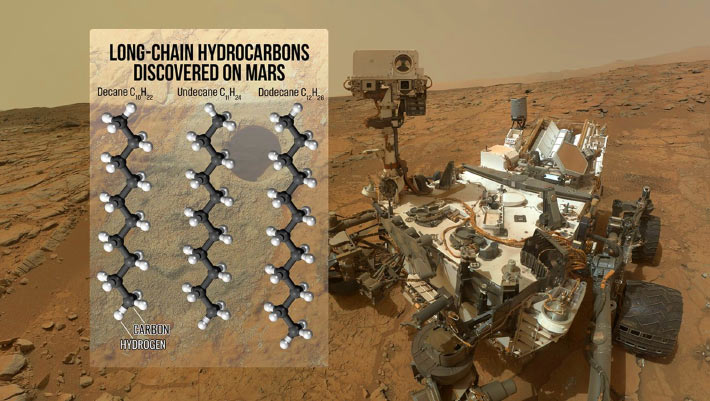
Sarkar’s group developed electronic gadgets made from biocompatible polymer and metal layers produced on silicon wafers utilizing a basic CMOS procedure. “We made the gadgets this little with lithography, the method utilized in making transistors for chips in our computer systems,” Sarkar describes. They were approximately 200 nanometers thick and 10 microns in size– that kept them subcellular, because a monocyte cell typically determines in between 12 and 18 microns. The gadgets were triggered and powered by infrared light at a wavelength that might permeate numerous centimeters into the brain.
As soon as the gadgets were produced and removed the wafer, the next thing to determine was connecting them to monocytes.
To do this, the group covered the surface areas of the electronic gadgets with dibezocyclooctyne, a really reactive particle that can quickly connect to other chemicals, specifically nitrogen substances called azides. Sarkar and her associates chemically customized monocytes to put azides on their surface areas. In this manner, the electronic devices and cells might rapidly snap together, practically like Lego blocks (this technique, called click chemistry, got the 2022 Nobel Prize in chemistry).
The resulting service of cell-electronics hybrids was created to be biocompatible and might be injected into the circulatory system. This is why Sarkar called her principle “circulatronics.”
Naturally, Sarkar’s “circulatronic” hybrids fall a bit except sci-fi dreams, because they aren’t precisely actual nanobots. They might be the closest thing we’ve developed so far.
Synthetic nerve cells
To evaluate these hybrids in live mice, the scientists prepared a fluorescent variation to make them simpler to track. Mice were anesthetized initially, and the group synthetically produced swelling at a particular place in their brains, around the ventrolateral thalamic nucleus. The hybrids were injected into the veins of the mice. After approximately 72 hours, the time researchers anticipated would be required for the monocytes to reach the swelling, Sarkar and her coworkers began running tests.
It ended up that the majority of the injected hybrids reached their location in one piece– the electronic devices mainly stayed connected to the monocytes. The group’s measurements recommend that around 14,000 hybrids handled to effectively implant themselves near the nerve cells in the target location of the brain. In action to infrared irradiation, they triggered substantial neuronal activation, similar to standard electrodes implanted by means of surgical treatment.
The genuine strength of the hybrids, Sarkar believes, is the method they can be tuned to particular illness. “We selected monocytes for this experiment due to the fact that swelling areas in the brain are typically the target in lots of neurodegenerative illness,” Sarkar states. Depending upon the application, however, the hybrids’ efficiency can be changed by controling their electronic and cellular elements. “We have actually currently checked utilizing mesenchymal stem cells for the Alzheimer’s, or T cells and other neural stem cells for growths,” Sarkar describes.
She went on to state that her innovation one day might assist with positioning the implants in brain areas that today can not be securely reached through surgical treatment. “There is a brain cancer called glioblastoma that forms diffused growth websites. Another example is DIPG [a form of glioma]which is a terminal brain cancer in kids that establishes in an area where surgical treatment is difficult,” she includes.
In the more far-off future, the hybrids can discover applications beyond targeting illness. The majority of the research studies that have actually depended on information from brain implants were restricted to individuals who experienced serious brain conditions. The implants were put in their brains for healing factors, and taking part in research study tasks was something they simply concurred to do on the side.
Since the electronic devices in Sarkar’s hybrids can be created to completely deteriorate after a set time, the group believes this might possibly allow them to collect brain implant information from healthy individuals– the implants would do their task throughout of the research study and be gone when it’s done. Unless we desire them to remain, that is.
“The ease of application can make the implants possible in brain-computer user interfaces developed for healthy individuals,” Sarkar argues. “Also, the electrodes can be made to work as synthetic nerve cells. In concept, we might improve ourselves– increase our neuronal density.”
However, the group desires to put the hybrids through a screening project on bigger animals and then get them FDA-approved for scientific trials. Through Cahira Technologies, an MIT spinoff business established to take the “circulatronics” innovation to the marketplace, Sarkar wishes to make this occur within the next 3 years.
Nature Biotechnology, 2025. DOI: 10.1038/ s41587-025-02809-3
Jacek Krywko is a freelance science and innovation author who covers area expedition, expert system research study, computer technology, and all sorts of engineering wizardry.
31 Comments
Learn more
As an Amazon Associate I earn from qualifying purchases.